Nano Intellects 2025
Peers Alley Media,Canada

Primary goal of attending an international conference is to present a paper to the experts and influencers. It gives you a platform to exchange your interest-related thoughts, paving the way for possible future collaborations.

Use this platform to build connections with an elite group of wise men and women to enhance your intellect. Young entrepreneurs, this is a great platform to connect with your peers.

Knowledge is Power. Knowledge teaches skills. Skills define excellence. Use this platform to become cognizant of your interest area to achieve excellence in your domain.

Attending a conference give you opportunity to get your abstract or paper published in conference proceedings

Meet and greet a myriad of industry professionals and academia experts with common interest. Every meal will be an opportunity to meet and interact with fellow researchers, attendees and experts.

Expand your professional competency and learn useful tips and tricks of your industry in our skill-building workshops.

Explore insights on recent advancements, new equipment, new techniques, and unpublished data, learn from thought-leaders and get to network with a great line up of speakers.

Our exhibits floor offers the attendees with a dynamic display of the latest products with cutting-edge technology.

Investing in you is the best investment. Peers Alley conferences give the patrons with a feeling of the serendipity of real learning, skill development in strategic workshops, networking and start-up opportunities, thus, is value for money.

Attending the conference gives you much needed break from your regular duties. It also allows you to explore new cities, culture and meet new people. You will feel energized and rejuvenated to return to the university and continue with the job after attending the conference.
Conferences are vital forum for academic researchers and business leaders. "It involves multiple presentations, interactive breakout sessions, hands-on product demonstrations and unrivalled networking opportunities".
We have invited some of the world's most sought-after keynote speakers, experts, brand ambassadors, and industry leaders to share their thoughts and ideas with our conference guests.
Register Now
The global pain management market is significant and growing market, with an estimated value of around USD 62.6 billion in 2020. The market is expected to continue to grow at a CAGR of around 4.9% from 2021 to 2028, driven by factors such as the increasing prevalence of chronic pain, an aging population, and the introduction of new pain management products and therapies.
The future of pain medicine research is very promising and exciting. Advances in technology, neuroscience, and other fields are opening up new avenues for developing more effective and targeted treatments for pain. Some of the key areas of research in pain medicine that are likely to have a significant impact in the future include: Precision medicine, neuroimaging, digital health, regenerative medicine and alternative therapies.
Here Adv. Pain Med 2023 plays a crucial role in bringing the latest innovations and therapeutic approaches from the bench to the bedside. This conference is critical in identifying emerging trends and advancements in the field and in translating these discoveries into practical applications that can benefit patients.
Dear participants and esteemed guests,
It is my great pleasure to welcome you to the Euro-Global Congress on Advanced Therapeutics in Pain Medicine and Pain Management to be held from Septmeber 12-13, 2023 in London, UK.
Pain is a complex and multifaceted phenomenon that affects millions of people worldwide, and managing it effectively requires a multidisciplinary approach. This congress aims to bring together researchers, clinicians and experts from various disciplines to discuss the latest advances in pain medicine, including new therapies and interventions, best practices, and emerging trends. Through this congress, we hope to foster productive discussions and collaborations that will contribute to improving patient outcomes and advancing the field of pain medicine.
The congress program includes keynote speeches, distinguished speaker talks, oral presentations and workshops covering a broad range of topics related to advanced therapeutics and procedures for pain management. We are confident that the congress will offer a platform for exchanging ideas, discussing new developments, and sharing experiences.
On behalf of the organizing committee, I would like to extend our sincere thanks to all the participants and sponsors for their invaluable contributions to the congress. We look forward to your active participation and fruitful discussions.
With best regards,
Adv. Pain Med 2023
Organizing Committee
Peers Alley Media, Canada

Children’s National Hospital, USA

University of Bologna, Italy

Stanford University, USA

Federal University, Brazil

Pain measurement and assessment is the process of evaluating the intensity, duration, location, and quality of pain experienced by an individual. It is a crucial component of pain management and helps healthcare providers develop effective treatment plans for their patients.
Here are some common methods used for pain measurement and assessment:
Self-Report: This is the most common method of pain assessment. Patients are asked to rate their pain using a scale, usually from 0 to 10, where 0 represents no pain and 10 represents the worst pain imaginable.
Visual Analog Scale (VAS): This is a type of self-report where patients are asked to mark their pain level on a 10 cm line, with one end representing no pain and the other end representing the worst pain imaginable.
Numeric Rating Scale (NRS): This is another type of self-report where patients are asked to rate their pain using a number from 0 to 10, where 0 represents no pain and 10 represents the worst pain imaginable.
Verbal Rating Scale (VRS): This is a self-report where patients are asked to describe their pain using words, such as mild, moderate, or severe.
Wong-Baker FACES Pain Rating Scale: This is a visual self-report where patients are shown a series of faces with different expressions, and asked to point to the face that best represents their pain.
Behavioral Observation: This method involves observing the patient's behavior, such as facial expressions, body movements, and vocalizations, to assess their pain level.
Physiological Measures: This method involves measuring physiological changes in the patient's body, such as heart rate, blood pressure, and skin conductance, to assess their pain level.
It's important to note that pain is subjective and can be influenced by many factors, such as culture, age, and gender. Therefore, healthcare providers should use a combination of methods to get a comprehensive understanding of their patient's pain.
Tags
Pain Medicine Conferences 2023 Europe
Anaesthesia and Critical Care Conferences
Pain Management and Palliative Care Conferences
Alternative Medicine Conferences
Cancer Pain Conferences
Peers Alley Media Scholars Opinion
Pain Management Conferences 2023
Chronic Pain Syndromes Conferences
Pain Medicine Conferences 2023
Physical Medicine Meetings 2023
Anaesthesia Meetings Europe

Pharmacotherapy, or the use of drugs, is an important component of pain management. There are several classes of drugs that can be used for pain relief, each with its own unique mechanism of action and potential side effects.
Here are some of the most common pharmacotherapeutic drugs used in pain management:
Nonsteroidal Anti-inflammatory Drugs (NSAIDs): These drugs work by reducing inflammation, which can cause pain. Common NSAIDs include aspirin, ibuprofen, and naproxen.
Acetaminophen: This drug is a common pain reliever that works by blocking pain signals in the brain. It is often used to treat mild to moderate pain.
Opioids: These drugs are often used for severe pain and work by binding to opioid receptors in the brain and spinal cord, reducing the perception of pain. Examples include morphine, fentanyl, and oxycodone.
Antidepressants: Certain antidepressants, such as tricyclic antidepressants and selective serotonin and norepinephrine reuptake inhibitors (SSNRIs), can be effective in treating chronic pain. They work by altering the levels of neurotransmitters in the brain that are involved in pain perception.
Anticonvulsants: Certain anticonvulsant drugs, such as gabapentin and pregabalin, can be effective in treating neuropathic pain. They work by reducing the sensitivity of nerves that transmit pain signals.
Local anesthetics: These drugs can be used to block pain signals from specific areas of the body. Examples include lidocaine and bupivacaine.
It's important to note that all drugs have potential side effects, and the use of these drugs should always be closely monitored by a healthcare provider. Additionally, pharmacotherapy is just one component of pain management, and other interventions such as physical therapy, psychological therapy, and alternative therapies may also be used to manage pain.
Tags
Headache Conferences
Acute Pain Management Conferences
Pain Management Conferences 2023
Cancer Pain Conferences
Alternative Medicine Conferences
Pain Medicine Conferences
Chronic Pain Syndromes Conferences
Physical Medicine Meetings 2023
Osteoporosis Meetings 2023 USA
Pain Medicine Conferences 2023
Pain medicine and anesthesia are two related fields that are involved in the management of pain in different settings. While both fields involve the use of drugs to manage pain, they differ in their approach and scope. Here are some key differences between pain medicine and anesthesia:
Focus: Pain medicine focuses on the diagnosis and management of chronic and acute pain conditions, while anesthesia is primarily concerned with the administration of drugs to produce a loss of sensation and consciousness during medical procedures.
Treatment Modalities: Pain medicine uses a variety of treatment modalities to manage pain, including medications, physical therapy, psychological therapy, and interventional procedures such as nerve blocks and epidural injections. Anesthesia primarily uses drugs to produce anesthesia and sedation during medical procedures.
Types of Pain: Pain medicine deals with a wide range of pain conditions, including chronic pain, neuropathic pain, and cancer pain, among others. Anesthesia is primarily concerned with acute pain, which is pain that occurs suddenly and is usually related to a medical procedure or surgery.
Administration: Pain medicine is often administered in an outpatient setting, while anesthesia is usually administered in a hospital or surgical center by an anesthesiologist.
Despite these differences, pain medicine and anesthesia often work together to manage pain in patients undergoing surgery or other medical procedures. Anesthesiologists may use a variety of techniques to manage pain during and after surgery, such as nerve blocks and epidural injections, while pain medicine specialists may provide ongoing management of chronic pain conditions.
Tags
Surgical Pain Management Conferences
Cancer Pain Conferences
Osteoporosis Meetings 2023 USA
Physical Medicine Meetings 2023
Pain Medicine Conferences 2023
Pain Medicine Conferences 2023 Europe
Acute Pain Management Conferences
Pain Management and Palliative Care Conferences
Peers Alley Media Scholars Opinion
Pain Medicine Conferences
Headache Conferences
Anaesthesia Meetings Europe
Pain Management Conferences 2023

Advanced Interventional Pain Management (AIPM) is a sub-specialty of pain management that focuses on the use of minimally invasive procedures to diagnose and treat various types of pain. These procedures are performed under fluoroscopy or ultrasound guidance, and often involve the use of needles, catheters, and other instruments to access and treat specific pain generators.
Some of the most common AIPM procedures include:
Epidural steroid injections - this procedure involves the injection of a steroid medication into the epidural space to reduce inflammation and relieve pain.
Facet joint injections - this procedure involves the injection of a steroid medication into the small joints between the vertebrae of the spine to reduce inflammation and relieve pain.
Radiofrequency ablation - this procedure involves the use of radiofrequency energy to heat and destroy nerve fibers that are transmitting pain signals.
Spinal cord stimulation - this procedure involves the implantation of a small device that sends electrical impulses to the spinal cord to block pain signals.
Sympathetic nerve blocks - this procedure involves the injection of a local anesthetic around the sympathetic nerves to relieve pain.
AIPM is typically performed by pain management specialists who have received advanced training in interventional pain management techniques. These specialists work closely with other healthcare providers to develop individualized treatment plans for patients with chronic pain conditions, such as back pain, neck pain, joint pain, and nerve pain.
AIPM procedures are generally safe and well-tolerated, and can provide significant pain relief for many patients. However, like any medical procedure, they do carry some risks and potential side effects, which should be carefully discussed with the patient prior to the procedure.
Tags
Pain Medicine Conferences 2023
Pain Management Conferences 2023
Pain Medicine Conferences 2023 Europe
Anaesthesia and Critical Care Conferences
Pain Management and Palliative Care Conferences
Acute Pain Management Conferences
Pain Medicine Conferences
Surgical Pain Management Conferences
Headache Conferences
Cancer Pain Conferences
Anesthesia and Critical Care are two closely related medical specialties that are essential for the care of patients undergoing surgery or experiencing life-threatening medical conditions.
Anesthesia involves the administration of medications to induce a temporary loss of sensation or consciousness for the purpose of performing surgical procedures, as well as for pain management during and after surgery. Anesthesiologists are physicians who specialize in the use of these medications, and they work closely with the surgical team to ensure the patient's safety and comfort throughout the procedure.
Critical Care, on the other hand, involves the management of life-threatening medical conditions, such as severe infections, respiratory failure, and heart failure. Critical care specialists, also known as intensivists, provide advanced life support and monitoring for critically ill patients in intensive care units (ICUs) or other specialized units. They also work closely with other healthcare providers to develop and implement treatment plans tailored to each patient's individual needs.
The overlap between Anesthesia and Critical Care is particularly important in the management of patients undergoing complex surgeries or experiencing multiple organ failure. Anesthesiologists with specialized training in Critical Care are known as Critical Care Anesthesiologists, and they play a critical role in the management of patients in the ICU. They are responsible for monitoring the patient's vital signs, managing mechanical ventilation, administering medications, and coordinating care with other members of the healthcare team.
In summary, Anesthesia and Critical Care are two closely related medical specialties that are essential for the safe and effective management of patients undergoing surgery or experiencing life-threatening medical conditions. The collaboration between Anesthesiologists and Critical Care specialists is vital for ensuring the best possible outcomes for these patients.
Tags
Headache Conferences
Physical Medicine Meetings 2023
Osteoporosis Meetings 2023 USA
Pain Medicine Conferences 2023 Europe
Chronic Pain Syndromes Conferences
Anaesthesia and Critical Care Conferences
Alternative Medicine Conferences
Pain Management and Palliative Care Conferences
Peers Alley Media Scholars Opinion
Osteoporosis Meetings 2023 USA
Surgical Pain Management Conferences

Pain management and palliative care are two medical specialties that are closely related and both focus on improving the quality of life of patients who are experiencing pain or other distressing symptoms.
Pain management is a medical specialty that focuses on the diagnosis and treatment of pain. Pain specialists work to identify the underlying causes of pain and develop a comprehensive treatment plan that may include medication management, physical therapy, behavioral therapy, interventional procedures, and other modalities to manage pain.
Palliative care, on the other hand, is a multidisciplinary approach to care that focuses on relieving the symptoms and improving the quality of life of patients who have serious or life-threatening illnesses. Palliative care specialists work to address physical, emotional, and spiritual needs of patients and their families, and provide support throughout the course of the illness.
Both pain management and palliative care may involve the use of medications to manage pain and other symptoms. However, the goals of treatment differ between the two specialties. Pain management focuses on reducing or eliminating pain, while palliative care aims to improve quality of life by managing pain and other symptoms while addressing the emotional and spiritual needs of the patient and their family.
In some cases, patients may receive both pain management and palliative care simultaneously. For example, a patient with advanced cancer may receive palliative care to manage their symptoms and improve their quality of life, while also receiving pain management to treat the pain associated with their cancer.
In summary, pain management and palliative care are two closely related medical specialties that focus on improving the quality of life of patients who are experiencing pain or other distressing symptoms. While the goals of treatment differ between the two specialties, they may be used together to provide comprehensive care for patients with serious or life-threatening illnesses.
Tags
Pain Management Conferences 2023
Peers Alley Media Scholars Opinion
Osteoporosis Meetings 2023 USA
Acute Pain Management Conferences
Headache Conferences
Pain Management and Palliative Care Conferences
Anaesthesia Meetings Europe
Pain Relief Conferenes
Alternative Medicine Conferences
Surgical Pain Management Conferences
Chronic Pain Syndromes Conferences
Physical Medicine Meetings 2023

Chronic pain syndromes are conditions that are characterized by persistent pain that lasts for several months or longer. These conditions can be caused by a wide range of underlying medical conditions, including musculoskeletal disorders, neuropathic pain, cancer, and autoimmune disorders.
Some common examples of chronic pain syndromes include:
Back pain: This is one of the most common chronic pain syndromes, affecting millions of people worldwide. Back pain can be caused by a variety of underlying conditions, such as herniated discs, degenerative disc disease, spinal stenosis, and osteoarthritis.
Fibromyalgia: This is a condition that is characterized by widespread musculoskeletal pain, fatigue, and sleep disturbances. The cause of fibromyalgia is unknown, but it is believed to be related to abnormal processing of pain signals in the brain and changes in neurotransmitters.
Neuropathic pain: This is a type of pain that is caused by damage to the nerves. It is often described as burning, shooting, or stabbing pain, and can be caused by conditions such as diabetes, shingles, and nerve damage from surgery or trauma.
Complex regional pain syndrome: This is a condition that typically affects an arm or a leg and is characterized by severe pain, swelling, and changes in skin color and temperature. The cause of complex regional pain syndrome is not fully understood.
Headaches: Chronic headaches can be caused by a variety of underlying conditions, such as tension headaches, migraines, and cluster headaches.
Treatment of chronic pain syndromes typically involves a multidisciplinary approach that may include medication management, physical therapy, psychological counseling, and interventional procedures, such as nerve blocks and spinal cord stimulation. The goal of treatment is to improve quality of life and function, reduce pain and other symptoms, and help patients manage their condition over the long-term.
Tags
Anaesthesia Meetings Europe
Headache Conferences
Pain Relief Conferenes
Chronic Pain Syndromes Conferences
Pain Medicine Conferences
Surgical Pain Management Conferences
Peers Alley Media Scholars Opinion
Cancer Pain Conferences
Pain Medicine Conferences 2023 Europe
Osteoporosis Meetings 2023 USA
Alternative Medicine Conferences
Pain Medicine Conferences 2023
Pain management is an essential component of the overall management of rheumatological diseases, which are conditions that affect the joints, bones, and muscles. These diseases are often chronic and can cause significant pain and disability, affecting the patient's quality of life.
Common rheumatological diseases include osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and lupus. The goals of pain management in rheumatological diseases are to reduce pain and inflammation, improve function and mobility, and enhance the patient's overall quality of life.
The treatment of pain in rheumatological diseases often involves a combination of pharmacological and non-pharmacological interventions. Pharmacological interventions may include:
Nonsteroidal anti-inflammatory drugs (NSAIDs): These medications are often used to reduce pain and inflammation in rheumatological diseases. NSAIDs can be taken orally or applied topically.
Disease-modifying antirheumatic drugs (DMARDs): These medications are used to modify the course of the disease and reduce inflammation. DMARDs may take several weeks or months to be effective.
Biologic drugs: These are a type of DMARD that are used to target specific components of the immune system that are responsible for causing inflammation.
Analgesics: These medications are used to relieve pain, and may include acetaminophen, opioids, or other pain medications.
Non-pharmacological interventions may include:
Physical therapy: This can include exercises to improve strength and flexibility, as well as modalities such as heat or cold therapy.
Occupational therapy: This may involve the use of adaptive equipment or modifications to the patient's environment to improve function and reduce pain.
Cognitive-behavioral therapy: This may involve relaxation techniques or other psychological interventions to help patients cope with pain and improve their overall well-being.
In summary, pain management is an important part of the overall management of rheumatological diseases. Treatment often involves a combination of pharmacological and non-pharmacological interventions, with the goal of reducing pain and inflammation, improving function and mobility, and enhancing the patient's overall quality of life.
Tags
Headache Conferences
Anaesthesia Meetings Europe
Alternative Medicine Conferences
Pain Medicine Conferences 2023 Europe
Pain Management and Palliative Care Conferences
Anaesthesia and Critical Care Conferences
Osteoporosis Meetings 2023 USA
Pain Relief Conferenes
Acute Pain Management Conferences
Pain Management Conferences 2023
Pain Medicine Conferences 2023
Surgical Pain Management Conferences
Osteoporosis Meetings 2023 USA

Pain management in the elderly can be challenging due to age-related changes in physiology, increased risk of adverse effects from medications, and the presence of comorbid conditions. It is important to recognize that chronic pain is not a normal part of aging and that it can have a significant impact on the elderly person's quality of life.
The following are some key considerations for pain management in the elderly:
Assessment: Accurate assessment of pain is essential in order to develop an effective treatment plan. In the elderly, pain assessment may be complicated by cognitive impairment, language barriers, or communication difficulties. Pain assessment tools specifically designed for use in the elderly population may be helpful.
Pharmacological management: Medications are often the first line of treatment for chronic pain in the elderly. However, the use of medications should be carefully monitored to avoid potential adverse effects. Lower doses of medications may be necessary due to age-related changes in pharmacokinetics and pharmacodynamics.
Non-pharmacological management: Non-pharmacological interventions, such as physical therapy, occupational therapy, acupuncture, and relaxation techniques, may be effective in reducing pain in the elderly population. These interventions may be particularly beneficial for those who are unable to tolerate medications or who have multiple comorbid conditions.
Multidisciplinary approach: A multidisciplinary approach to pain management, involving healthcare providers from different specialties, may be particularly effective in the elderly population. This approach may include a combination of pharmacological and non-pharmacological interventions, as well as psychological support and social services.
Education: Education about pain management is important for both the elderly person and their caregivers. This may include information about medication management, non-pharmacological interventions, and strategies for coping with pain.
In summary, pain management in the elderly requires a multidisciplinary approach that takes into account the unique needs and challenges of this population. Accurate assessment of pain, careful monitoring of medications, and the use of non-pharmacological interventions may be particularly beneficial. Education about pain management is also important for both the elderly person and their caregivers.
Tags
Pain Medicine Conferences 2023 Europe
Pain Relief Conferenes
Osteoporosis Meetings 2023 USA
Alternative Medicine Conferences
Pain Management Conferences 2023
Pain Medicine Conferences
Chronic Pain Syndromes Conferences
Acute Pain Management Conferences
Osteoporosis Meetings 2023 USA
Anaesthesia and Critical Care Conferences
Headache Conferences
Anaesthesia Meetings Europe

Physical Medicine and Rehabilitation (PM&R) is a medical specialty that focuses on the prevention, diagnosis, and treatment of disabilities related to the musculoskeletal system, as well as other medical conditions that affect the function of the body. PM&R physicians, also known as physiatrists, work with patients of all ages and medical backgrounds to improve their physical function, reduce pain, and enhance their quality of life.
Some of the key areas of focus for PM&R include:
Rehabilitation after injury or illness: PM&R physicians work with patients who have experienced physical injury or illness, such as stroke or traumatic brain injury, to help them regain physical function and independence.
Pain management: PM&R physicians are trained to manage chronic pain, including back pain, joint pain, and neuropathic pain, through a variety of interventions, including physical therapy, medication management, and interventional procedures.
Sports medicine: PM&R physicians are trained in the diagnosis and treatment of sports-related injuries, and work with athletes to help them recover from injuries and improve their performance.
Occupational medicine: PM&R physicians work with individuals who have work-related injuries or conditions to help them return to work and regain their physical function.
Geriatric rehabilitation: PM&R physicians work with older adults to address age-related conditions, such as osteoporosis and arthritis, and to help them maintain their independence and quality of life.
The treatment options available to PM&R physicians vary depending on the individual patient and their specific condition. Some common interventions may include physical therapy, occupational therapy, medication management, interventional procedures such as injections or nerve blocks, and assistive devices such as braces or prostheses.
Overall, PM&R is a specialized field that focuses on helping individuals with disabilities or physical impairments to improve their physical function and enhance their quality of life.
Tags
Osteoporosis Meetings 2023 USA
Anaesthesia and Critical Care Conferences
Physical Medicine Meetings 2023
Alternative Medicine Conferences
Pain Medicine Conferences 2023 Europe
Pain Management Conferences 2023
Chronic Pain Syndromes Conferences
Pain Medicine Conferences
Peers Alley Media Scholars Opinion
Pain Medicine Conferences 2023
Anaesthesia Meetings Europe
Cancer Pain Conferences
Acute Pain Management Conferences

Complementary and Alternative Medicine (CAM) refers to a diverse group of healthcare practices, treatments, and products that are not considered part of conventional or mainstream medicine. These practices and treatments are often used alongside, or in place of, conventional medical therapies.
Some examples of CAM practices include acupuncture, herbal medicine, chiropractic, massage therapy, meditation, and yoga. CAM therapies may be used to treat a wide range of conditions, including chronic pain, anxiety, depression, and digestive disorders.
While some CAM practices have been well-studied and have shown efficacy in treating certain conditions, others have not been scientifically validated or may even be harmful. The effectiveness of CAM practices can be difficult to evaluate due to the lack of rigorous scientific studies and the variability of individual responses to treatments.
It is important for individuals considering CAM therapies to inform their healthcare providers and to thoroughly research the therapy they are considering. Some CAM practices may interact with conventional medications or may be contraindicated for certain conditions. Additionally, individuals should be aware that some CAM therapies may not be covered by insurance.
While CAM therapies can be appealing to individuals seeking alternative or holistic approaches to healthcare, it is important to approach these treatments with caution and to make informed decisions about their use. Healthcare providers can work with their patients to help them navigate the use of CAM therapies alongside conventional treatments and to evaluate the potential benefits and risks of these therapies.
Tags
Alternative Medicine Conferences
Pain Management and Palliative Care Conferences
Cancer Pain Conferences
Pain Relief Conferenes
Pain Medicine Conferences
Anaesthesia Meetings Europe
Pain Medicine Conferences 2023
Acute Pain Management Conferences
Surgical Pain Management Conferences
Peers Alley Media Scholars Opinion
Pain Medicine Conferences 2023 Europe
Pain Management Conferences 2023

Cancer pain refers to any pain experienced by a person with cancer. Cancer pain can be caused by the cancer itself, the treatments used to manage the cancer, or other medical conditions that may be present along with cancer.
Cancer pain can be acute or chronic, mild or severe, and can range from a dull ache to a sharp, stabbing pain. Some people experience intermittent pain, while others have continuous pain. The type of pain experienced can depend on various factors, such as the location of the cancer, the stage of the cancer, and the individual's pain threshold.
There are many ways to manage cancer pain, and the treatment options depend on the individual's specific situation. Pain management may include medication, such as opioids or nonsteroidal anti-inflammatory drugs (NSAIDs), nerve blocks or other interventional procedures, physical therapy, relaxation techniques, or other complementary therapies.
It is important for people with cancer to communicate with their healthcare team about any pain they are experiencing. By working together, they can develop a pain management plan that takes into account the individual's specific needs and preferences while minimizing any side effects or risks associated with the treatment.
Tags
Peers Alley Media Scholars Opinion
Physical Medicine Meetings 2023
Pain Medicine Conferences 2023 Europe
Pain Management and Palliative Care Conferences
Acute Pain Management Conferences
Pain Management Conferences 2023
Pain Relief Conferenes
Surgical Pain Management Conferences
Pain Medicine Conferences 2023
Headache Conferences
Chronic Pain Syndromes Conferences
Anaesthesia Meetings Europe

Surgical pain management refers to the various techniques and strategies used to control pain after surgery. Surgical pain can be acute, meaning it is short-term and lasts for a few days to a few weeks, or chronic, meaning it persists for more than three months after the surgical procedure.
There are several methods of surgical pain management that can be used alone or in combination. These include:
Medications: Pain medications such as opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and acetaminophen can be used to manage post-surgical pain.
Regional Anesthesia: Regional anesthesia techniques like epidurals or nerve blocks can be used to numb a specific area of the body and reduce pain.
Patient-controlled analgesia (PCA): PCA involves the use of a computerized pump that allows patients to self-administer pain medication within safe limits.
Non-pharmacological approaches: Non-pharmacological approaches such as massage, relaxation techniques, or acupuncture can be used to manage pain and reduce the need for medications.
Enhanced Recovery After Surgery (ERAS): ERAS is a multimodal approach that combines various techniques and interventions, such as preoperative education, opioid-sparing medications, and early ambulation, to reduce surgical stress and promote rapid recovery.
The choice of surgical pain management approach depends on the type and duration of surgery, patient factors such as age and medical history, and surgeon preference. Effective pain management after surgery is essential to promote healing, reduce complications, and improve the overall patient experience.
Tags
Pain Management and Palliative Care Conferences
Physical Medicine Meetings 2023
Anaesthesia Meetings Europe
Alternative Medicine Conferences
Acute Pain Management Conferences
Pain Medicine Conferences
Anaesthesia and Critical Care Conferences
Chronic Pain Syndromes Conferences
Pain Relief Conferenes
Pain Medicine Conferences 2023 Europe

Opioids are a class of medications that are commonly used to treat pain. They work by binding to specific receptors in the brain and spinal cord, reducing the perception of pain. Opioids can be natural, synthetic, or semi-synthetic, and they are often used for moderate to severe pain relief.
Commonly used opioids include morphine, codeine, oxycodone, hydrocodone, and fentanyl, among others. These medications are available in various forms, including tablets, capsules, patches, injections, and suppositories.
While opioids are effective in managing pain, they are also associated with several side effects, such as constipation, nausea, dizziness, sedation, respiratory depression, and addiction. Long-term use of opioids can also lead to tolerance, dependence, and withdrawal symptoms when the medication is discontinued.
Due to the potential for abuse and addiction, opioids are subject to strict prescribing guidelines and are typically used only for short-term pain management or for patients with chronic pain who have not responded to other treatments.
It is important for patients taking opioids to follow their healthcare provider's instructions carefully, to use the medication only as directed, and to avoid sharing or selling their medication to others. Regular monitoring, including assessments for potential misuse or abuse, can also help to minimize the risks associated with opioid use.
Tags
Headache Conferences
Anaesthesia and Critical Care Conferences
Pain Management Conferences 2023
Anaesthesia Meetings Europe
Osteoporosis Meetings 2023 USA
Alternative Medicine Conferences
Peers Alley Media Scholars Opinion
Acute Pain Management Conferences
Pain Medicine Conferences 2023
Antidepressants and anticonvulsants are medications that are commonly used in the treatment of various medical conditions, including depression, anxiety, neuropathic pain, and seizures.
Antidepressants are medications that are primarily used to treat depression, but they can also be used to manage other conditions such as anxiety disorders, chronic pain, and migraines. They work by increasing the levels of certain neurotransmitters, such as serotonin and norepinephrine, in the brain. Some commonly used classes of antidepressants include selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants (TCAs).
Anticonvulsants, also known as antiepileptic drugs, are medications used to treat seizures or convulsions. They work by stabilizing the electrical activity in the brain and reducing the risk of seizures. However, anticonvulsants are also used to manage other conditions, including neuropathic pain and mood disorders such as bipolar disorder. Some commonly used anticonvulsants include gabapentin, pregabalin, carbamazepine, and valproic acid.
Both antidepressants and anticonvulsants can have side effects, including drowsiness, dizziness, and nausea. However, they are generally considered to have a lower risk of dependence and addiction compared to opioids. These medications may take several weeks to achieve their full effect and should be taken as prescribed by a healthcare provider.
It is important for patients taking antidepressants or anticonvulsants to communicate with their healthcare provider about any side effects or concerns they may have. Regular monitoring and dose adjustments may be necessary to ensure optimal treatment outcomes.
Tags
Pain Medicine Conferences 2023
Pain Medicine Conferences
Pain Management and Palliative Care Conferences
Surgical Pain Management Conferences
Anaesthesia Meetings Europe
Cancer Pain Conferences
Chronic Pain Syndromes Conferences
Pain Relief Conferenes
Alternative Medicine Conferences
Pain Management Conferences 2023
Osteoporosis Meetings 2023 USA
Acute Pain Management Conferences

Regenerative medicine is a field of medicine that focuses on harnessing the body's natural ability to heal and regenerate damaged or diseased tissues and organs. This field utilizes a variety of techniques, including stem cell therapy, tissue engineering, and gene therapy, to promote tissue regeneration and repair.
Stem cell therapy involves using stem cells to replace damaged or diseased cells or tissues. Stem cells have the ability to develop into different types of cells in the body, which makes them valuable in regenerating tissues that have been damaged due to injury or disease. There are different types of stem cells, including embryonic stem cells, adult stem cells, and induced pluripotent stem cells.
Tissue engineering involves growing replacement tissues or organs in a laboratory setting. This technique involves using a combination of cells, biomaterials, and growth factors to create tissues that can be transplanted into the body to replace damaged or diseased tissues.
Gene therapy involves using genes to treat or prevent disease. This technique involves introducing a healthy gene into the body to replace or supplement a faulty or missing gene that is causing a disease.
Regenerative medicine has the potential to revolutionize the treatment of many diseases and conditions, including heart disease, diabetes, neurodegenerative disorders, and cancer. However, more research is needed to fully understand the safety and effectiveness of these techniques.
It is important to note that not all regenerative medicine techniques are approved by regulatory agencies, and patients should always consult with a healthcare provider before undergoing any experimental treatments.
Tags
Headache Conferences
Pain Relief Conferenes
Cancer Pain Conferences
Osteoporosis Meetings 2023 USA
Alternative Medicine Conferences
Pain Management Conferences 2023
Pain Medicine Conferences 2023 Europe
Acute Pain Management Conferences
Pain Medicine Conferences 2023
Chronic Pain Syndromes Conferences

Osteoporosis is a condition characterized by a loss of bone density, which makes bones weaker and more prone to fractures. It is often called the "silent disease" because there are typically no symptoms until a fracture occurs. Osteoporosis can affect both men and women, but it is more common in women after menopause.
There are several risk factors that can increase the likelihood of developing osteoporosis, including age, gender, family history, low calcium and vitamin D intake, smoking, excessive alcohol consumption, and certain medical conditions or medications.
Treatment for osteoporosis typically involves a combination of lifestyle modifications and medications. Lifestyle modifications include regular exercise, a balanced diet with adequate calcium and vitamin D intake, and avoiding smoking and excessive alcohol consumption.
Medications used to treat osteoporosis include bisphosphonates, which help to slow down bone loss, and hormone therapy, which can help to prevent bone loss in women after menopause. Other medications that may be used include calcitonin, denosumab, and teriparatide.
Preventing osteoporosis is an important aspect of managing this condition. This can be achieved through regular exercise, maintaining a healthy diet, getting enough calcium and vitamin D, avoiding smoking and excessive alcohol consumption, and undergoing regular bone density screenings.
If you are at risk for osteoporosis or have been diagnosed with the condition, it is important to work with a healthcare provider to develop an individualized treatment plan that is tailored to your specific needs.
Tags
Physical Medicine Meetings 2023
Osteoporosis Meetings 2023 USA
Pain Management and Palliative Care Conferences
Pain Medicine Conferences
Peers Alley Media Scholars Opinion
Chronic Pain Syndromes Conferences
Osteoporosis Meetings 2023 USA
Headache Conferences
Pain Medicine Conferences 2023 Europe
Alternative Medicine Conferences
Pain Management Conferences 2023

Acute pain is a type of pain that is typically sudden in onset and is often caused by an injury, surgery, or a medical condition. Acute pain management is focused on providing relief for this type of pain, with the goal of minimizing discomfort and promoting healing.
The management of acute pain typically involves a multimodal approach that may include the use of medication, physical therapy, and other non-pharmacologic treatments.
Medications commonly used for the management of acute pain include nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, opioids, and local anesthetics. NSAIDs and acetaminophen are often used for mild to moderate pain, while opioids are reserved for more severe pain that is not responsive to other medications. Local anesthetics, such as lidocaine, can be used to provide targeted pain relief to a specific area.
Physical therapy and other non-pharmacologic treatments can also be effective in managing acute pain. These may include ice or heat therapy, massage, acupuncture, relaxation techniques, and cognitive-behavioral therapy.
It is important to work closely with a healthcare provider to develop an individualized treatment plan for acute pain management. This may involve adjusting the dose or type of medication used, as well as incorporating non-pharmacologic treatments. It is also important to follow any instructions provided by healthcare providers regarding medication use, as well as to report any side effects or concerns.
In some cases, acute pain may be an indication of a more serious underlying condition, and prompt medical attention may be necessary. If you experience severe or persistent pain, it is important to seek medical attention.
Tags
Pain Management Conferences 2023
Chronic Pain Syndromes Conferences
Anaesthesia and Critical Care Conferences
Anaesthesia Meetings Europe
Peers Alley Media Scholars Opinion
Surgical Pain Management Conferences
Pain Medicine Conferences 2023
Pain Medicine Conferences
Alternative Medicine Conferences
Acute Pain Management Conferences
Physical Medicine Meetings 2023
Nonsteroidal anti-inflammatory drugs (NSAIDs) are a group of medications commonly used to treat pain, fever, and inflammation. They work by blocking the production of certain chemicals in the body called prostaglandins, which are responsible for causing pain, swelling, and inflammation.
NSAIDs are available over-the-counter and by prescription, and can be used to treat a variety of conditions, including headache, menstrual cramps, muscle aches, arthritis, and other types of pain.
Common examples of NSAIDs include aspirin, ibuprofen, naproxen, diclofenac, and meloxicam. These medications can be taken orally, topically (as a cream or gel), or injected.
While NSAIDs are generally safe and effective when used as directed, they can have side effects, particularly when used long-term or in high doses. Common side effects may include stomach upset, nausea, diarrhea, and heartburn. More serious side effects may include stomach ulcers or bleeding, kidney problems, and increased risk of heart attack or stroke.
To minimize the risk of side effects, it is important to take NSAIDs only as directed, and to follow any instructions provided by a healthcare provider or on the medication label. People who are at increased risk for certain side effects, such as those with a history of stomach ulcers or heart disease, may need to avoid NSAIDs or use them with caution.
NSAIDs should also be used with caution in certain populations, including elderly individuals, those with kidney disease or liver disease, and pregnant women. In some cases, alternative pain management strategies may be recommended.
It is important to talk to a healthcare provider before starting any new medication, including NSAIDs, to discuss potential risks and benefits, and to determine the most appropriate treatment plan for your individual needs.
Tags
Headache Conferences
Osteoporosis Meetings 2023 USA
Surgical Pain Management Conferences
Pain Relief Conferenes
Alternative Medicine Conferences
Anaesthesia Meetings Europe
Chronic Pain Syndromes Conferences
Cancer Pain Conferences
Acute Pain Management Conferences
Physical Medicine Meetings 2023
Osteoporosis Meetings 2023 USA
Peers Alley Media Scholars Opinion
Radiography and imaging play an important role in pain medicine by helping healthcare providers to diagnose and treat conditions that cause pain. These imaging techniques allow healthcare providers to visualize internal structures and identify any abnormalities that may be causing pain.
Common imaging techniques used in pain medicine include X-rays, computed tomography (CT) scans, magnetic resonance imaging (MRI) scans, and ultrasound.
X-rays use a small amount of radiation to create images of bones and other structures inside the body. They are often used to diagnose fractures, dislocations, and other bone-related injuries or conditions.
CT scans use a series of X-rays to create detailed images of the inside of the body. They are often used to diagnose conditions that affect the bones, joints, and internal organs.
MRI scans use a magnetic field and radio waves to create images of the inside of the body. They are often used to diagnose conditions that affect soft tissues, such as muscles, ligaments, and organs.
Ultrasound uses high-frequency sound waves to create images of internal structures. It is often used to diagnose conditions that affect the muscles, tendons, and other soft tissues.
In pain medicine, these imaging techniques can help healthcare providers to identify the underlying cause of pain, such as a herniated disc or arthritis. They can also help to guide certain pain management procedures, such as injections or nerve blocks.
While these imaging techniques are generally safe and non-invasive, they do expose the patient to radiation or strong magnetic fields, and may not be appropriate for all individuals. It is important to discuss any potential risks and benefits of imaging with a healthcare provider, and to follow any instructions provided for preparing for the procedure.
Tags
Pain Relief Conferenes
Pain Medicine Conferences
Anaesthesia Meetings Europe
Osteoporosis Meetings 2023 USA
Surgical Pain Management Conferences
Acute Pain Management Conferences
Chronic Pain Syndromes Conferences
Cancer Pain Conferences
Pain Management and Palliative Care Conferences
Osteoporosis Meetings 2023 USA
Peers Alley Media Scholars Opinion

Headache is a common condition that affects people of all ages and backgrounds. There are many different types of headaches, each with their own specific causes, symptoms, and treatments.
Some common types of headaches include:
Tension headaches: These are the most common type of headache, and are often described as a dull, aching pain that affects both sides of the head. They can be caused by stress, poor posture, or tension in the neck and shoulders.
Migraines: These headaches are typically characterized by a throbbing pain on one side of the head, and may be accompanied by other symptoms such as sensitivity to light, nausea, and vomiting.
Cluster headaches: These headaches are rare, but can be very painful. They typically occur in cycles, with frequent attacks of severe pain on one side of the head.
Sinus headaches: These headaches are often caused by inflammation or infection of the sinuses, and are typically accompanied by symptoms such as facial pain and pressure, congestion, and post-nasal drip.
Treatment for headaches depends on the underlying cause and type of headache. For tension headaches, over-the-counter pain relievers such as acetaminophen or ibuprofen may be effective, along with stress management techniques such as relaxation or meditation. For migraines, specific medications such as triptans or preventive medications may be prescribed, along with lifestyle changes such as avoiding triggers and maintaining a regular sleep schedule. For cluster headaches, certain medications such as oxygen therapy or nerve blocks may be recommended.
It is important to talk to a healthcare provider if you experience frequent or severe headaches, as they may be a sign of an underlying medical condition that requires treatment.
Tags
Pain Medicine Conferences 2023 Europe
Cancer Pain Conferences
Chronic Pain Syndromes Conferences
Alternative Medicine Conferences
Acute Pain Management Conferences
Pain Medicine Conferences
Anaesthesia Meetings Europe
Osteoporosis Meetings 2023 USA
Pain Relief Conferenes
Physical Medicine Meetings 2023
Anaesthesia and Critical Care Conferences
Peers Alley Media Scholars Opinion

Muscle and myofascial pain are common conditions that can cause discomfort and limited mobility. Muscle pain can be caused by a variety of factors, including overuse, injury, tension, and poor posture. Myofascial pain syndrome is a chronic pain disorder that affects the muscles and surrounding connective tissue (fascia).
Symptoms of muscle and myofascial pain may include:
Treatment for muscle and myofascial pain may involve a combination of approaches, including:
Pain relievers: Over-the-counter pain relievers such as acetaminophen or ibuprofen may be effective in reducing pain and inflammation.
Physical therapy: A physical therapist can provide exercises and stretches to improve muscle strength, flexibility, and range of motion, as well as massage and other techniques to relieve tension and promote healing.
Trigger point injections: These are injections of anesthetic or anti-inflammatory medications into specific trigger points (knots of muscle) that are causing pain and discomfort.
Heat or ice therapy: Applying heat or cold to the affected area can help to reduce inflammation and relieve pain.
Relaxation techniques: Techniques such as deep breathing, meditation, or yoga can help to reduce stress and tension in the muscles.
It is important to talk to a healthcare provider if you experience frequent or severe muscle or myofascial pain, as they may be a sign of an underlying medical condition that requires treatment. A healthcare provider can help to determine the underlying cause of the pain and develop an appropriate treatment plan.
Tags
Acute Pain Management Conferences
Pain Relief Conferenes
Pain Medicine Conferences 2023 Europe
Pain Medicine Conferences
Anaesthesia and Critical Care Conferences
Physical Medicine Meetings 2023
Pain Management Conferences 2023
Alternative Medicine Conferences
Cancer Pain Conferences
Headache Conferences
Chronic Pain Syndromes Conferences
Anaesthesia Meetings Europe
Osteoporosis Meetings 2023 USA
Surgical Pain Management Conferences
Osteoporosis Meetings 2023 USA

Neck and shoulder pain is a common condition that can be caused by a variety of factors, including poor posture, injury, overuse, and stress. The pain may be localized to the neck or shoulder area, or may radiate down the arm or into the upper back.
Symptoms of neck and shoulder pain may include:
Pain or stiffness in the neck or shoulder area
Limited range of motion or difficulty moving the affected area
Headaches
Tingling or numbness in the arm or hand
Muscle spasms or cramps
Treatment for neck and shoulder pain may involve a combination of approaches, including:
Pain relievers: Over-the-counter pain relievers such as acetaminophen or ibuprofen may be effective in reducing pain and inflammation.
Physical therapy: A physical therapist can provide exercises and stretches to improve muscle strength, flexibility, and range of motion, as well as massage and other techniques to relieve tension and promote healing.
Heat or ice therapy: Applying heat or cold to the affected area can help to reduce inflammation and relieve pain.
Posture correction: Maintaining good posture while sitting, standing, and sleeping can help to reduce strain on the neck and shoulders.
Relaxation techniques: Techniques such as deep breathing, meditation, or yoga can help to reduce stress and tension in the muscles.
In some cases, more advanced treatment options such as injections or surgery may be recommended, especially if the pain is severe or chronic. It is important to talk to a healthcare provider if you experience frequent or severe neck and shoulder pain, as they may be a sign of an underlying medical condition that requires treatment.
Tags
Pain Medicine Conferences 2023 Europe
Pain Management and Palliative Care Conferences
Pain Relief Conferenes
Acute Pain Management Conferences
Alternative Medicine Conferences
Surgical Pain Management Conferences
Osteoporosis Meetings 2023 USA
Physical Medicine Meetings 2023
Peers Alley Media Scholars Opinion
Anaesthesia Meetings Europe
Pain Management Conferences 2023
Headache Conferences

Back pain is a common condition that can be caused by a variety of factors, including poor posture, injury, overuse, and underlying medical conditions such as herniated discs, osteoarthritis, or spinal stenosis. The pain may be localized to the back or may radiate down the legs.
Symptoms of back pain may include:
Treatment for back pain may involve a combination of approaches, including:
Pain relievers: Over-the-counter pain relievers such as acetaminophen or ibuprofen may be effective in reducing pain and inflammation.
Physical therapy: A physical therapist can provide exercises and stretches to improve muscle strength, flexibility, and range of motion, as well as massage and other techniques to relieve tension and promote healing.
Heat or ice therapy: Applying heat or cold to the affected area can help to reduce inflammation and relieve pain.
Posture correction: Maintaining good posture while sitting, standing, and sleeping can help to reduce strain on the back.
Relaxation techniques: Techniques such as deep breathing, meditation, or yoga can help to reduce stress and tension in the muscles.
In some cases, more advanced treatment options such as injections or surgery may be recommended, especially if the pain is severe or chronic. It is important to talk to a healthcare provider if you experience frequent or severe back pain, as they may be a sign of an underlying medical condition that requires treatment.
Tags
Cancer Pain Conferences
Pain Medicine Conferences 2023
Pain Medicine Conferences
Peers Alley Media Scholars Opinion
Surgical Pain Management Conferences
Pain Management and Palliative Care Conferences
Chronic Pain Syndromes Conferences
Anaesthesia Meetings Europe
Physical Medicine Meetings 2023
Pain Management Conferences 2023
Pain Medicine Conferences 2023 Europe
Headache Conferences
Anaesthesia and Critical Care Conferences
Acute Pain Management Conferences

Visceral pain is pain that originates from the internal organs, such as the stomach, intestines, liver, and kidneys. Visceral pain can be caused by a variety of factors, including inflammation, infection, ischemia (lack of blood flow), or stretching of the organ wall. Visceral pain may be difficult to localize and may be felt in different parts of the body, depending on the organ involved.
Symptoms of visceral pain may include:
Treatment for visceral pain depends on the underlying cause and may involve a combination of approaches, including:
Medications: Pain relievers and anti-inflammatory drugs may be effective in reducing pain and inflammation.
Nerve blocks: Injecting a local anesthetic or steroid into the nerves that supply the affected organ can help to reduce pain and inflammation.
Physical therapy: A physical therapist can provide exercises and stretches to improve muscle strength, flexibility, and range of motion, as well as massage and other techniques to relieve tension and promote healing.
Relaxation techniques: Techniques such as deep breathing, meditation, or yoga can help to reduce stress and tension in the body and may help to reduce visceral pain.
It is important to talk to a healthcare provider if you experience frequent or severe visceral pain, as they may be a sign of an underlying medical condition that requires treatment.
Tags
Osteoporosis Meetings 2023 USA
Chronic Pain Syndromes Conferences
Headache Conferences
Osteoporosis Meetings 2023 USA
Acute Pain Management Conferences
Pain Medicine Conferences 2023
Pain Management Conferences 2023
Physical Medicine Meetings 2023
Pain Medicine Conferences 2023 Europe
Alternative Medicine Conferences
Chronic urogenital and pelvic pain is a condition characterized by pain or discomfort in the pelvic region, which may be felt in the lower abdomen, groin, or genital area. Chronic urogenital and pelvic pain can be caused by a variety of factors, including infection, inflammation, nerve damage, or muscular dysfunction. It may also be associated with conditions such as interstitial cystitis, endometriosis, or pelvic floor dysfunction.
Symptoms of chronic urogenital and pelvic pain may include:
Treatment for chronic urogenital and pelvic pain depends on the underlying cause and may involve a combination of approaches, including:
Medications: Pain relievers, muscle relaxants, and antidepressants may be effective in reducing pain and improving mood.
Physical therapy: A physical therapist can provide exercises and stretches to improve muscle strength, flexibility, and range of motion, as well as massage and other techniques to relieve tension and promote healing.
Nerve blocks: Injecting a local anesthetic or steroid into the nerves that supply the affected area can help to reduce pain and inflammation.
Behavioral therapy: Techniques such as cognitive behavioral therapy (CBT) may help to reduce anxiety and improve coping skills.
Surgery: In some cases, surgery may be recommended to remove adhesions or other sources of pain.
It is important to talk to a healthcare provider if you experience chronic urogenital and pelvic pain, as they may be a sign of an underlying medical condition that requires treatment.
Tags
Pain Relief Conferenes
Headache Conferences
Osteoporosis Meetings 2023 USA
Pain Medicine Conferences
Acute Pain Management Conferences
Peers Alley Media Scholars Opinion
Physical Medicine Meetings 2023
Anaesthesia Meetings Europe
Chronic Pain Syndromes Conferences
Surgical Pain Management Conferences
Pain Management Conferences 2023
Pain Management and Palliative Care Conferences

Pain in pregnancy is common and can be caused by a variety of factors, including hormonal changes, weight gain, and changes in posture. In some cases, pain in pregnancy can be a sign of a more serious condition and should be evaluated by a healthcare provider.
Here are some common causes of pain in pregnancy:
Back pain: As the uterus expands, it can cause strain on the muscles and ligaments in the lower back, leading to pain and discomfort.
Round ligament pain: The round ligaments support the uterus and stretch as it grows, causing pain in the lower abdomen or groin area.
Pelvic pain: As the body prepares for childbirth, the pelvic joints may become more relaxed and can cause pain or discomfort.
Braxton Hicks contractions: These are mild contractions that can occur throughout pregnancy and can cause discomfort or pain in the abdomen.
Headaches: Hormonal changes and increased blood flow can cause headaches during pregnancy.
Treatment for pain in pregnancy may include:
Exercise: Regular exercise can help to strengthen the muscles and improve posture, reducing the risk of back and pelvic pain.
Heat or cold therapy: Applying heat or cold to the affected area can help to reduce pain and inflammation.
Massage: Gentle massage can help to relieve muscle tension and promote relaxation.
Medications: Some pain medications, such as acetaminophen, may be safe to use during pregnancy. However, it is important to consult with a healthcare provider before taking any medication during pregnancy.
Rest: Taking breaks and getting adequate rest can help to reduce pain and fatigue during pregnancy.
It is important to discuss any pain or discomfort during pregnancy with a healthcare provider to rule out any serious underlying conditions and to ensure the safety of both the mother and the baby.
Tags
Anaesthesia and Critical Care Conferences
Alternative Medicine Conferences
Pain Medicine Conferences
Cancer Pain Conferences
Pain Medicine Conferences 2023 Europe
Osteoporosis Meetings 2023 USA
Surgical Pain Management Conferences
Chronic Pain Syndromes Conferences
Peers Alley Media Scholars Opinion
Headache Conferences
Pain Management and Palliative Care Conferences
Pain Relief Conferenes

Neuropathic pain is a type of chronic pain caused by damage or dysfunction of the nervous system. It is a complex and often debilitating condition that can result from a variety of underlying conditions, including diabetes, cancer, multiple sclerosis, and nerve injuries.
The symptoms of neuropathic pain can vary widely and may include:
Treatment for neuropathic pain often involves a combination of approaches, including:
Medications: Antidepressants, anticonvulsants, and other medications may be effective in reducing nerve pain.
Topical treatments: Creams, gels, or patches containing lidocaine or capsaicin may provide relief for localized pain.
Nerve blocks: Injecting a local anesthetic or steroid into the nerves that supply the affected area can help to reduce pain and inflammation.
Physical therapy: Exercises and stretches to improve muscle strength, flexibility, and range of motion may be helpful in reducing pain and improving function.
Transcutaneous electrical nerve stimulation (TENS): This therapy involves the use of a device that sends electrical impulses to the affected area, which may help to reduce pain.
Cognitive-behavioral therapy (CBT): Techniques such as relaxation training and guided imagery may help to reduce stress and anxiety, which can contribute to neuropathic pain.
It is important to work with a healthcare provider to develop an individualized treatment plan for neuropathic pain. This may involve a trial-and-error approach to find the most effective combination of treatments for each individual.
Tags
Pain Management Conferences 2023
Headache Conferences
Physical Medicine Meetings 2023
Osteoporosis Meetings 2023 USA
Pain Medicine Conferences 2023 Europe
Surgical Pain Management Conferences
Cancer Pain Conferences
Acute Pain Management Conferences
Anaesthesia and Critical Care Conferences
Anaesthesia Meetings Europe

Pain in infants, children, and adolescents is a complex and often challenging issue. Children may not be able to express their pain in the same way as adults, and healthcare providers must rely on a variety of cues to assess and manage pain in this population.
Here are some common types of pain in infants, children, and adolescents:
Acute pain: Acute pain is usually caused by an injury or illness and is typically short-lived. Examples include postoperative pain, headache, or pain associated with medical procedures.
Chronic pain: Chronic pain is pain that persists for more than 3 months and can be caused by conditions such as juvenile arthritis, sickle cell disease, or cancer.
Procedural pain: Procedural pain is pain associated with medical procedures such as injections, blood draws, or dressing changes.
Phantom pain: Phantom pain is pain that is felt in a body part that has been amputated or removed.
Managing pain in infants, children, and adolescents may involve a combination of approaches, including:
Non-pharmacologic therapies: Distraction techniques, relaxation techniques, and guided imagery may be helpful in reducing pain and anxiety.
Pharmacologic therapies: Medications such as acetaminophen or ibuprofen may be used to relieve pain in children. In some cases, stronger medications such as opioids may be necessary.
Local anesthetics: Topical anesthetics such as lidocaine or EMLA cream may be used to numb the skin before medical procedures.
Nerve blocks: Injecting a local anesthetic or steroid into the nerves that supply the affected area can help to reduce pain and inflammation.
Physical therapy: Exercises and stretches to improve muscle strength, flexibility, and range of motion may be helpful in reducing pain and improving function.
It is important to work with a healthcare provider to develop an individualized treatment plan for pain in infants, children, and adolescents. This may involve a combination of therapies tailored to the individual child's needs and preferences.
Tags
Acute Pain Management Conferences
Pain Relief Conferenes
Pain Medicine Conferences 2023
Pain Medicine Conferences
Anaesthesia and Critical Care Conferences
Headache Conferences
Pain Management Conferences 2023
Cancer Pain Conferences
Osteoporosis Meetings 2023 USA
Anaesthesia Meetings Europe
Osteoporosis Meetings 2023 USA
Pain Management and Palliative Care Conferences
Pain relief in individuals with substance use and addictive disorders can be challenging as they may have a history of substance abuse or dependence, and some pain medications can be addictive. Therefore, it is important to approach pain management in these individuals with caution and a multidisciplinary team approach involving pain specialists, addiction specialists, and mental health professionals.
Here are some approaches to pain relief in individuals with substance use and addictive disorders:
Non-opioid medications: Non-opioid medications such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to manage pain in these individuals. These medications have a lower risk of addiction and can be effective for managing mild to moderate pain.
Opioid-sparing medications: Medications that can be used to reduce the amount of opioids needed to manage pain may be considered. These may include adjuvant analgesics such as antidepressants or anticonvulsants.
Opioid therapy: If opioids are necessary for pain management, a careful assessment of the individual's risk of addiction should be conducted. The lowest effective dose should be used, and the individual should be closely monitored for signs of addiction or misuse.
Behavioral interventions: Cognitive-behavioral therapy (CBT) and other behavioral interventions may be helpful in managing pain and reducing the risk of addiction. These interventions can help individuals to develop coping skills and improve their ability to manage pain without relying on opioids.
Addiction treatment: Individuals with substance use disorders may benefit from addiction treatment, such as medication-assisted treatment (MAT) or counseling. These treatments can help to reduce the risk of relapse and improve overall outcomes.
It is important to work with a healthcare provider who has experience in managing pain in individuals with substance use and addictive disorders. An individualized treatment plan should be developed based on the individual's specific needs and preferences.
Tags
Chronic Pain Syndromes Conferences
Anaesthesia and Critical Care Conferences
Alternative Medicine Conferences
Peers Alley Media Scholars Opinion
Acute Pain Management Conferences
Pain Medicine Conferences 2023
Pain Relief Conferenes
Surgical Pain Management Conferences
Cancer Pain Conferences
Physical Medicine Meetings 2023
Headache Conferences
Pain Management Conferences 2023

Psychological treatment can be a valuable component of pain management, as it can help individuals to better understand and cope with their pain. Here are some common psychological treatments used in pain management:
Cognitive-behavioral therapy (CBT): CBT is a type of therapy that focuses on changing negative thought patterns and behaviors that may be contributing to pain. This can include techniques such as relaxation training, cognitive restructuring, and behavioral activation.
Acceptance and Commitment Therapy (ACT): ACT is a type of therapy that helps individuals to develop acceptance of their pain while also identifying and committing to values-based goals. This can include techniques such as mindfulness, acceptance, and values clarification.
Biofeedback: Biofeedback involves using electronic devices to monitor and provide feedback on physiological responses such as muscle tension and heart rate. This can help individuals to learn to control their physical responses to pain and reduce pain-related distress.
Hypnotherapy: Hypnotherapy involves using hypnosis to help individuals to manage their pain. This can include techniques such as relaxation, guided imagery, and suggestion therapy.
Mindfulness-based interventions: Mindfulness-based interventions involve teaching individuals to pay attention to the present moment in a non-judgmental way. This can help to reduce pain-related distress and improve overall well-being.
Psychological treatment can be used alone or in combination with other pain management approaches, such as medication and physical therapy. It is important to work with a healthcare provider who is knowledgeable about psychological treatments for pain management to develop an individualized treatment plan.
Tags
Peers Alley Media Scholars Opinion
Acute Pain Management Conferences
Osteoporosis Meetings 2023 USA
Alternative Medicine Conferences
Headache Conferences
Anaesthesia Meetings Europe
Cancer Pain Conferences
Osteoporosis Meetings 2023 USA
Physical Medicine Meetings 2023
Pain Relief Conferenes
Pain Medicine Conferences
Pain Medicine Conferences 2023 Europe
Pain Management and Palliative Care Conferences

Psychiatric treatment can be an important component of pain management, particularly for individuals who are experiencing significant emotional distress related to their pain.
Here are some common psychiatric treatments used in pain management:
Medications: Antidepressants, anticonvulsants, and other medications commonly used in psychiatry may also be effective in managing pain, particularly neuropathic pain. These medications can help to reduce pain intensity and improve mood and sleep.
Psychiatric counseling: Psychiatric counseling can help individuals to address emotional and psychological factors that may be contributing to their pain, such as depression, anxiety, and trauma. This can include individual therapy, group therapy, or family therapy.
Mind-body interventions: Mind-body interventions such as yoga, tai chi, and meditation can be effective in managing pain and reducing emotional distress. These interventions can help individuals to relax, reduce muscle tension, and increase feelings of well-being.
Transcranial Magnetic Stimulation (TMS): TMS is a non-invasive brain stimulation technique that can be used to manage pain by stimulating certain areas of the brain. This can help to reduce pain intensity and improve overall well-being.
Electroconvulsive Therapy (ECT): ECT is a type of brain stimulation therapy that can be effective in managing severe pain, particularly in individuals who have not responded to other treatments. ECT involves passing a small electrical current through the brain to produce a controlled seizure.
It is important to work with a healthcare provider who is knowledgeable about psychiatric treatments for pain management to develop an individualized treatment plan. A multidisciplinary approach that includes both psychiatric and non-psychiatric treatments may be most effective for managing pain in individuals with significant emotional distress.
Tags
Anaesthesia and Critical Care Conferences
Pain Relief Conferenes
Surgical Pain Management Conferences
Osteoporosis Meetings 2023 USA
Pain Medicine Conferences 2023
Chronic Pain Syndromes Conferences
Osteoporosis Meetings 2023 USA
Pain Medicine Conferences 2023 Europe
Headache Conferences
Pain Medicine Conferences
Anaesthesia Meetings Europe
Acute Pain Management Conferences
Pain Management and Palliative Care Conferences
Alternative Medicine Conferences

Sex and gender issues can play an important role in the experience and management of pain. Here are some key considerations:
Women are more likely to experience chronic pain than men. This may be due to differences in hormones, anatomy, and physiology.
Women may experience different types of pain than men. For example, women are more likely to experience pain related to reproductive organs, such as menstrual cramps and endometriosis.
Women and men may respond differently to pain medications. For example, women may require higher doses of opioids than men to achieve the same level of pain relief.
There may be differences in pain perception and expression between men and women. Women may be more likely to report pain and seek medical attention, while men may be more likely to try to "tough it out" or downplay their pain.
Gender identity and sexual orientation can also impact pain management. For example, transgender individuals may have unique pain management needs related to hormone therapy and gender affirmation surgeries.
It is important for healthcare providers to be aware of these sex and gender-related issues in pain management and to provide individualized care that takes into account each patient's unique needs and experiences. This may include tailoring pain management approaches based on sex and gender, as well as providing education and support to help individuals better understand and manage their pain.
Tags
Pain Medicine Conferences 2023
Osteoporosis Meetings 2023 USA
Pain Medicine Conferences 2023 Europe
Pain Relief Conferenes
Anaesthesia Meetings Europe
Osteoporosis Meetings 2023 USA
Acute Pain Management Conferences
Pain Management Conferences 2023
Headache Conferences
Peers Alley Media Scholars Opinion
Alternative Medicine Conferences
Chronic Pain Syndromes Conferences
Cancer Pain Conferences

Placebo refers to a treatment or substance that has no active therapeutic effect but is given to a patient with the intention of providing a psychological benefit, such as a reduction in symptoms or an improvement in subjective well-being. Placebos can be administered in various forms, including pills, injections, or even sham surgeries.
Pain is a complex experience that can be influenced by a variety of factors, including physiological, psychological, and social factors. Pain can be classified into two categories: acute pain and chronic pain. Acute pain is a sudden and sharp pain that lasts for a short period of time, while chronic pain persists for longer periods, often lasting for months or even years.
Studies have shown that placebos can have a significant impact on pain. The placebo effect is the phenomenon where patients experience a reduction in pain or other symptoms after receiving a placebo treatment. The exact mechanisms behind the placebo effect are not yet fully understood, but it is believed to involve the release of natural painkillers in the brain, such as endorphins.
One of the key factors that influence the effectiveness of a placebo treatment is the patient's expectation of its efficacy. If a patient believes that a treatment will be effective, they are more likely to experience a reduction in pain, even if the treatment has no active therapeutic effect. This suggests that psychological factors, such as the patient's beliefs and expectations, play an important role in the placebo effect.
In some cases, placebos can be a useful tool in the treatment of pain, particularly in situations where traditional pain management approaches are not effective or have significant side effects. However, it is important to note that placebos should not be used as a substitute for evidence-based treatments, and patients should always receive the most appropriate and effective treatment for their condition.
Tags
Chronic Pain Syndromes Conferences
Osteoporosis Meetings 2023 USA
Pain Relief Conferenes
Pain Management and Palliative Care Conferences
Anaesthesia and Critical Care Conferences
Cancer Pain Conferences
Pain Management Conferences 2023
Pain Medicine Conferences
Pain Medicine Conferences 2023 Europe
Surgical Pain Management Conferences
Physical Medicine Meetings 2023
Market Velue of Pain Medicine in USA
The market value of pain medicine in the USA is difficult to estimate precisely due to the complex nature of the healthcare system and the variety of products and treatments available. However, according to a report by Grand View Research, the global pain management market size was valued at USD 65.1 billion in 2020, with the North American region, including the USA, accounting for the largest share of the market.
The pain management market includes a wide range of products and treatments, including over-the-counter pain relievers, prescription pain medications, non-pharmacological therapies such as physical therapy and acupuncture, and surgical interventions for chronic pain conditions.
According to the Centers for Disease Control and Prevention (CDC), prescription opioids are one of the most commonly prescribed medications for pain in the USA. The CDC also reports that the economic burden of prescription opioid misuse in the USA was estimated to be $78.5 billion per year, including healthcare costs, lost productivity, and criminal justice involvement.
Overall, the market value of pain medicine in the USA is significant, reflecting the high prevalence of pain conditions and the importance of effective pain management in improving patient outcomes and quality of life. However, it is important to balance the benefits of pain management with the potential risks and harms of certain treatments, such as prescription opioids.
Market Velue of Pain Medicine in Europe
The pain medicine market in Europe is a significant and growing market. According to a report by ResearchAndMarkets, the European pain management therapeutics market was valued at €9.46 billion in 2020 and is projected to reach €13.16 billion by 2027, growing at a compound annual growth rate (CAGR) of 4.6% during the forecast period.
The growth of the pain medicine market in Europe is attributed to several factors, including the increasing prevalence of chronic pain conditions, such as arthritis and back pain, and the growing demand for effective pain management treatments.
The market is dominated by a few key players, including Pfizer, Eli Lilly, and Johnson & Johnson. These companies are investing heavily in research and development to develop new and innovative pain management therapies. Additionally, the market is witnessing an increase in mergers and acquisitions as companies seek to expand their product portfolios and strengthen their market position.
Overall, the pain medicine market in Europe is expected to continue to grow in the coming years, driven by the increasing prevalence of chronic pain conditions and the demand for effective pain management treatments.
Market Velue of Pain Medicine in Asia
The pain medicine market in Asia is expected to experience significant growth in the coming years due to various factors, such as the aging population, the increasing prevalence of chronic diseases, and the rising demand for pain management treatments. According to a report by Market Data Forecast, the Asia-Pacific pain management market is projected to grow at a compound annual growth rate (CAGR) of 8.3% from 2020 to 2025.
In terms of market size, Japan is currently the largest market for pain management in Asia, followed by China and South Korea. However, other countries in the region, such as India and Southeast Asian countries, are also expected to contribute to the growth of the market in the coming years.
The market for pain medicine in Asia is highly competitive, with both multinational pharmaceutical companies and local manufacturers competing for market share. Some of the leading players in the market include Pfizer, GlaxoSmithKline, Novartis, and Johnson & Johnson, among others.
It's important to note that market value of pain medicine in Asia can be influenced by various factors such as healthcare policies, regulatory environment, and local economic conditions. Therefore, the market outlook and trends can vary significantly across different countries in the region.
Market Velue of Pain Medicine in Middle East
The Middle East region has a growing demand for pain medicine due to the increasing prevalence of chronic diseases such as arthritis, cancer, and neuropathic pain. Additionally, the aging population in the region is expected to contribute to the growth of the pain medicine market.
The market for pain medicine in the Middle East is expected to grow in the coming years, driven by factors such as increasing healthcare expenditure, growing awareness about pain management, and the launch of new pain medications. The market is also expected to be influenced by the growing trend of self-medication and the availability of over-the-counter pain medications.
Several major pharmaceutical companies have a presence in the Middle East and offer a range of pain management products, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and topical analgesics. Some of the key players in the Middle East pain medicine market include Pfizer, Novartis, Sanofi, and GlaxoSmithKline.
It is important to note that the use of opioids for pain management has been a topic of concern in the Middle East due to the potential for abuse and addiction. As a result, there has been a growing focus on non-opioid pain management alternatives, such as NSAIDs and non-pharmacological approaches.
Overall, the market value of pain medicine in the Middle East is expected to continue to grow, driven by factors such as increasing healthcare expenditure, the aging population, and the launch of new pain medications. However, the market is also likely to be influenced by regulatory changes and evolving trends in pain management practices.
___________________________________________________________________________________________________________________________________________________________________________
List of pain medicine companies in USA
Pfizer / Johnson & Johnson / Merck & Co / AbbVie / Teva Pharmaceuticals / Endo Pharmaceuticals / Mallinckrodt Pharmaceuticals / Purdue Pharma / Mylan Pharmaceuticals / Novartis Pharmaceuticals /
List of pain medicine companies in Europe
Grünenthal / AstraZeneca / Pfizer / Boehringer Ingelheim / Teva Pharmaceutical Industries / Novartis / Sanofi / GlaxoSmithKline / Mundipharma / Eli Lilly and Company / Bayer / Johnson & Johnson / Merck KGaA / Abacus Medicine / Kyowa Kirin / Orion Corporation / Zambon / Fidia Farmaceutici / Viatris / Angelini Pharma / Almirall / Rottapharm Biotech / ProStrakan Group / Ethypharm / Menarini Group /
List of pain medicine companies in Asia
Takeda Pharmaceutical Company Limited (Japan) / Eisai Co., Ltd. (Japan) / Mitsubishi Tanabe Pharma Corporation (Japan) / Otsuka Pharmaceutical Co., Ltd. (Japan) / Astellas Pharma Inc. (Japan) / Hisamitsu Pharmaceutical Co., Inc. (Japan) / Yamanouchi Pharmaceutical Co., Ltd. (Japan) / Korea Pharma Co., Ltd. (South Korea) / Hwang's Pharmaceutical Co., Ltd. (South Korea) / CKD Bio Corporation (South Korea) / LG Life Sciences Ltd. (South Korea) / Nanjing Legend Biotech Co., Ltd. (China) / Jiangsu Hengrui Medicine Co., Ltd. (China) / China Resources Sanjiu Medical & Pharmaceutical Co., Ltd. (China) / Sinopharm Group Co., Ltd. (China) / Shanghai Fosun Pharmaceutical (Group) Co., Ltd. (China) / Zhejiang Hisun Pharmaceutical Co., Ltd. (China) / Simcere Pharmaceutical Group (China) / Torrent Pharmaceuticals Ltd. (India) / Dr. Reddy's Laboratories Ltd. (India) / Sun Pharmaceutical Industries Ltd. (India) / Lupin Limited (India) / Cipla Limited (India) / Glenmark Pharmaceuticals Ltd. (India) /
List of pain medicine companies in Middle East
Hikma Pharmaceuticals (Jordan) / Jamjoom Pharmaceuticals (Saudi Arabia) / Tabuk Pharmaceuticals Manufacturing Co. (Saudi Arabia) / Julphar (United Arab Emirates) / Neopharma (United Arab Emirates) / Medpharma (Jordan) / Al Hayat Pharmaceuticals (Jordan) / Pharma International Company (Jordan) / AstraZeneca Gulf (United Arab Emirates) / Pfizer Gulf (United Arab Emirates) / Sanofi Middle East (United Arab Emirates) / laxoSmithKline Middle East (United Arab Emirates) / Boehringer Ingelheim Middle East (United Arab Emirates) / Merck Serono Middle East (United Arab Emirates) / Novartis Middle East (United Arab Emirates) / AbbVie Middle East (United Arab Emirates) / Bayer Middle East (United Arab Emirates) / Roche Middle East (United Arab Emirates) / Eli Lilly Middle East (United Arab Emirates) / Janssen Middle East (United Arab Emirates) / Bristol Myers Squibb Middle East (United Arab Emirates) / Takeda Middle East (United Arab Emirates) / Biopharm (Syria) / Mega Pharma (Syria) / Abdi Ibrahim Global Pharma (Turkey) /
list of pain medicine societies in Europe
European Pain Federation (EFIC) / International Association for the Study of Pain (IASP) - European Chapter British Pain Society / French Society for the Study and Treatment of Pain (SFETD) / German Pain Society (DGSS) / Italian Society for the Study of Pain (SISD) / Scandinavian Association for the Study of Pain (SASP) / Spanish Society of Pain (SED) / Belgian Pain Society (SBSD) / Dutch Pain Society (NVP) / Austrian Pain Society (ÖSG) / Czech Pain Society (CPS) / Danish Pain Society (DPS) / Estonian Pain Society (EPS) / Finnish Pain Society (FIPS) / Hellenic Pain Society (HPS) / Hungarian Pain Society (HPS) / Irish Pain Society (IPS) / Latvian Association for the Study of Pain (LASP) / Lithuanian Association for the Study of Pain (LTLASP) / Norwegian Pain Society (NFS) / Polish Pain Society (PTB) / Portuguese Society for the Study of Pain (SPEdor) / Romanian Association for the Study and Treatment of Pain (RASTP) / Swedish Association for the Study of Pain (Svensk Smärtspecialistförening) /
list of Pain medicine societies in USA
American Academy of Pain Medicine (AAPM) / American Pain Society (APS) / International Association for the Study of Pain (IASP) - North American Chapter / American Society of Regional Anesthesia and Pain Medicine (ASRA) / American Society of Interventional Pain Physicians (ASIPP) / American Society of Pain and Neuroscience (ASPN) / American Chronic Pain Association (ACPA) / American Academy of Pain Management (AAPM) / American Society of Anesthesiologists (ASA) / American Board of Pain Medicine (ABPM) / American Society of Pain Educators (ASPE) / North American Neuromodulation Society (NANS) / Pain Society of the Carolinas (PSC) / Southern Pain Society (SPS) / Eastern Pain Association (EPA) / Western Pain Society (WPS) / Florida Academy of Pain Medicine (FAPM) / Georgia Pain and Wellness Center (GPWC) / Hawaii Pain Society (HPS) / Indiana Pain Society (IPS) / Michigan Pain Society (MPS) / New Jersey Society of Interventional Pain Physicians (NJSIPP) / New York State Pain Society (NYSPS) / Pennsylvania Pain Society (PPS) /
list of pain medicine societies in Asia
Asia Pacific Pain Association (APPA) / Korean Pain Society (KPS) / Japanese Pain Society (JPS) / Chinese Pain Society (CPS) / Indian Society for Study of Pain (ISSP) / Malaysian Association for the Study of Pain (MASP) / Indonesian Society of Regional Anesthesia and Pain Medicine (ISRAPM) / Philippine Society for Pain Medicine (PSPM) / Taiwan Society of Pain Medicine (TSPM) / Hong Kong Pain Society (HKPS) / Singapore Pain Society (SPS) / Thai Association for the Study of Pain (TASP) / Bangladesh Society for the Study of Pain (BSSP) / Sri Lanka Society for the Study of Pain (SLSSP) / Nepal Society for the Study of Pain (NSSP) / Pakistan Society for the Study of Pain (PSSP) / Vietnamese Society for the Study of Pain (VSSP) / Iranian Pain Society (IPS) / Israeli Pain Association (IPA) / Turkish Pain Society (TPS) / Jordanian Society for the Study of Pain (JSSP) / Saudi Pain Society (SPS) / Emirates Pain Society (EPS) / Iraqi Pain Society (IPS) / Lebanese Pain Society (LPS) /
list of pain medicine societies in Middle East
Iranian Pain Society (IPS) / Israeli Pain Association (IPA) / Turkish Pain Society (TPS) / Jordanian Society for the Study of Pain (JSSP) / Saudi Pain Society (SPS) / Emirates Pain Society (EPS) / Iraqi Pain Society (IPS) / Lebanese Pain Society (LPS) / Kuwait Pain Society (KPS) / Qatar Pain Society (QPS) / Bahrain Society for the Study and Treatment of Pain (BSSTP) / Oman Pain Society (OPS) / Yemen Pain Society (YPS) / Palestinian Pain Society (PPS) / Syrian Pain Society (SYPS) / Egyptian Society for Pain Management (ESPM) / Tunisian Society of Algology (STA) / Algerian Society of Algology and Pain Management (SAAAD) / Moroccan Society of Algology (SMA) / Libyan Society for Pain Medicine (LSPM) / Sudanese Society for Pain Medicine (SSPM) / Mauritanian Society of Pain Management (MSPM) / Djiboutian Society of Pain Management (DSPM) / Somali Society of Pain Management (SSPM) /
List of Best Pain Medicine Procedures
Epidural steroid injection / Facet joint injection / Radiofrequency ablation / Sympathetic nerve block / Trigger point injection / Spinal cord stimulation / Intrathecal drug delivery / Joint injection / Botox injection / Peripheral nerve block / Nerve conduction study / Transcranial magnetic stimulation / Sacroiliac joint injection / Discography / Peripheral nerve stimulation / Occipital nerve block / Ultrasound-guided injection / Lumbar sympathetic block / Stellate ganglion block / Pulsed radiofrequency / Neurolysis / Transforaminal epidural injection / Platelet-rich plasma injection / Ketamine infusion therapy / Intravenous regional anesthesia / Nerve root block / Celiac plexus block / Gasserian ganglion block / Suprascapular nerve block / Lumbar puncture / Lumbar epidural injection / Superior hypogastric plexus block / Median nerve block / Myofascial release / Sphenopalatine ganglion block / Piriformis injection / Greater occipital nerve block / Transcutaneous electrical nerve stimulation / Neuromodulation / Disc nucleoplasty / Disc decompression / Trigger point release / Endoscopic discectomy / Vertebral augmentation / Botulinum toxin type A injection / Perineural injection therapy / Interlaminar epidural injection / Lumbar radiofrequency neurotomy / Medial branch block / Occipital nerve stimulation / Sacral nerve stimulation / Gasserian rhizotomy / Ilioinguinal and iliohypogastric nerve block / Sympathectomy / Transforaminal lumbar interbody fusion / Arthroscopy / Intradiscal electrothermal therapy / Adhesiolysis / Pudendal nerve block / Joint arthroplasty / Intra-articular injection / Pulsed electromagnetic field therapy / Implantable intrathecal drug delivery system / Intercostal nerve block / Supraorbital nerve block / Hypogastric plexus block / Occipital nerve release / Rhizotomy / Epidural lysis of adhesions / Cryotherapy / Facet rhizotomy / Neuroplasty / Platelet-rich plasma therapy / Selective nerve root block / Transforaminal selective nerve root block / Stellate ganglion neurolysis / Cervical epidural injection / Joint fusion / Celiac plexus neurolysis / Ultrasound-guided nerve block / Carpal tunnel release / Intercostal muscle injection / Transverse abdominis plane block / Trigger point deactivation / Viscosupplementation injection / Iliohypogastric nerve block / Lumbar puncture with epidural blood patch / Tibial nerve stimulation / Sacral nerve root stimulation / Thoracic epidural injection / Paravertebral block / Trigger point acupuncture /
Contact us now and we will make your event unique & unforgettable
All numbers indicates percentage %
Europe
North America
Middle East
Asia Pacific
Africa
All numbers indicates percentage %
Pain Medicine Specialists and Physicians
Anesthesiologists
Neurologists & Psychiatrists
Physical Therapists & Occupational Therapist
Alternative Medicine Practitioners
Medical, Healthcare Students and Residents
Pain Researchers & Pain Researchers
Pharma & Biotech Companies

Objectives/Scope: Migraine-like headache symptoms are often-reported symptoms following a concussion (Lumba-Brown et al., 2019), resulting in a significant impact on the adolescent’s quality of life. Their self-efficacy for managing recovery-related stress and activity is hypothesized to be critical to managing headache pai
Objectives: Physical pain measurement can be analyzed by amygdala EEG current. These cranial nerve pain currents depend on the transport of ions such as glucose, dopamine, catechol, and epinephrine. Scope: Therefore, these ionic concentrations were analyzed by using voltammetry. Under optimal conditions, it was possible to det

Pain experienced by persons seeking voluntary assisted dying (VAD) has understandably been a principal driver ever since the concept of establishing such a service provision was first introduced in the Netherlands, Belgium, and the Northern Territories of Australia. Over the decades such a provision has now been advanced by a wo

In this talk, I offer a philosophical view and a conceptual analysis on some neurophysiological hypothesis on the role of interoception proper for mind and subjectivity grounding. I especially focus on ‘the feeling of being alive’. This feeling has attracted the attention of several scholars in different fields of the affe

Objective: This study aims to elucidate the association paths between melatonin and the learning and memory ability in drug-free patients with schizophrenia. Methods: A total of 108 schizophrenia patients and 109 healthy controls were enrolled in this study. Hopkins Verbal Learning Test-Revised and Brief Visuospatial Memory Test

A wave of heroin addiction hit Egypt by the early nineteen eighties. It became clear that the conventional medical and psychological methods need to be complimented by a peer based and therapeutic community approach if this challenge is to be met. The Freedom Drug Rehabilitation programme started in 1989 is believed to be one of

Background: Psychological/emotional abuse and neglect of children (PEA) has been a global issue. The significance of PEA can be illustrated by its prevalence of identified cases and evidence of its negative effects. However, there is diversity in how PEA is defined, and the meaning of PEA is unclear. Regardless, PEA could occur

Multiple sclerosis represents a debilitating disease. It has many different forms and warrants further investigation. The purpose of this research paper is to like at the available RNA sequencing for white matter lesion disorders in the brain. We performed a comprehensive systematic review to correlate RNA sequence to white matt
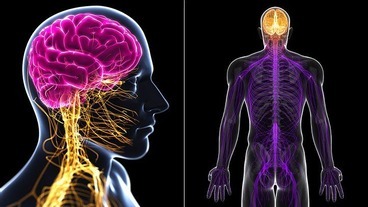
Introduction: We aimed to detect the causative gene in five unrelated families with recessive inheritance pattern neurological disorders involving the central nervous system, and the potential function of the NEMF gene in the central nervous system. Objective: This study aims to determine the genetic profile of individuals from